If you’re recently diagnosed with CML it can sometimes be difficult to take in all the information you’re given. Unfamiliar medical terms may be used that mean more to your doctor than to you, so you may end up not really processing everything that’s being said. You’re also likely to be given lots of different types of information in a short space of time, such as:
- scientific details about leukaemia and its treatments
- statistics about people with CML
- practical information about rights and responsibilities
- personal details about your appointment schedule and healthcare team
- test results and what terms like ‘cytogenetic response’ mean
If you feel overwhelmed by all this information, try to bear in mind that no-one expects you to take everything in straight away. If ever you’re in doubt, it’s better to ask and know for sure, than sit worrying. Healthcare professionals would rather know if there’s something bothering you, as they may be able to help.
A lot of people also get anxious when they’re in a hospital or at the doctor’s surgery, no matter how long they’ve had a particular condition. And when we’re anxious, communication can suffer. That’s why we’ve put together a few ideas about how you can get the most out of your medical appointments and come away feeling more informed.
Think ahead
It can help to prepare what you want to say in an appointment. Here on CML Life we have an appointment guide which can help you set out any questions you might have before each meeting with your doctor.
You could also set a goal for each appointment. This might be something like:
“I want to leave this appointment…
- …understanding my latest test results”
- …with some practical tips on managing fatigue and nausea”
- …understanding what my current medication is for and how it works”
Having a goal for the appointment can help keep the conversation on track, and make it more useful for you.
Come equipped
Take a friend: if there’s a friend or family member who can come with you to an appointment, it can be really handy to have another set of eyes and ears in the room with you. Your friend could take notes for you, leaving you free to concentrate on what the healthcare professional is telling you. It can also be useful to talk things over with your friend afterwards, to check that your understanding of what happened matches theirs.
Bring a pen and paper: you might find it helpful to note down things you might otherwise forget. You could also get your doctor or nurse to write down the technical terms they’re using so you can look them up later. Alternatively, you could use a voice recorder on your phone to have a record of the conversation, as memories can’t always be relied on.
Be confident
No matter how qualified and experienced your healthcare team might be, you are the expert in your own health, wellbeing and life. Be clear about what matters to you most, and remember that no-one can make decisions about you without your input or consent.
Ask open questions
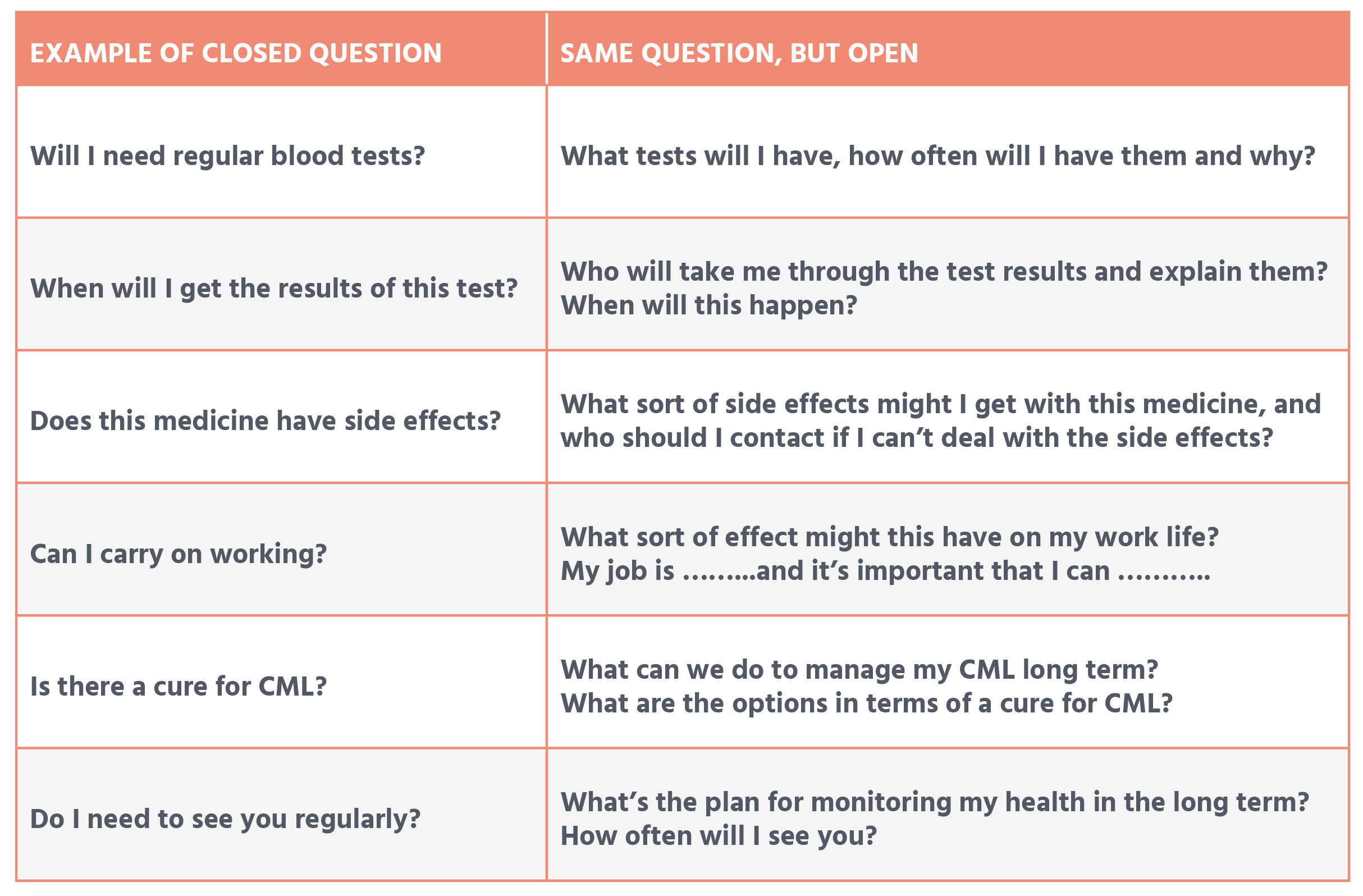
Asking open-ended questions can get a conversation going, which is more difficult with yes/no answers. Below on the left are some examples of ‘closed’ questions (short, exact answers), with ideas for more open questions on the right:
Be 100% sure about what’s being said
No-one likes feeling confused, or that they’re losing the thread of a conversation. If this happens, don’t be afraid to stop and ask questions to be sure you’ve got it. Could it be explained to you in another way? Before you leave, you could repeat back what you have understood from the conversation in your own words, so your doctor or nurse can better explain the details or fill in anything they’ve missed.
Say everything you want to say
If something’s bothering you, it’s worth telling your doctor or nurse about it. Don’t keep things back because it doesn’t seem relevant to the discussion, or you don’t know how to get the topic onto what you want to say. Even things that you may think are unrelated to CML may be relevant: your healthcare team could pick up a side effect or new symptom early, or they may be able to point you in the direction of a colleague who can help you better than they can.
Ask for help
Sometimes we all need a bit of help with something, whether that’s a kindly listening ear, medical advice or practical aid. If you need outside expertise or a helping hand, ask your healthcare team if they know of any help or support services in your area.
Next steps
Before you leave the doctor’s or nurse’s office, it can be good to agree with them what will happen next. That way, everyone is clear about what is going to happen and what, if anything, each of you needs to do before the next appointment. It can be part of helping you feel empowered and part of your own treatment plan.
Remember at any point, you can always assess how confident you feel in managing your health with our Health Confidence questionnaire.
